The best 7 ambient AI scribes
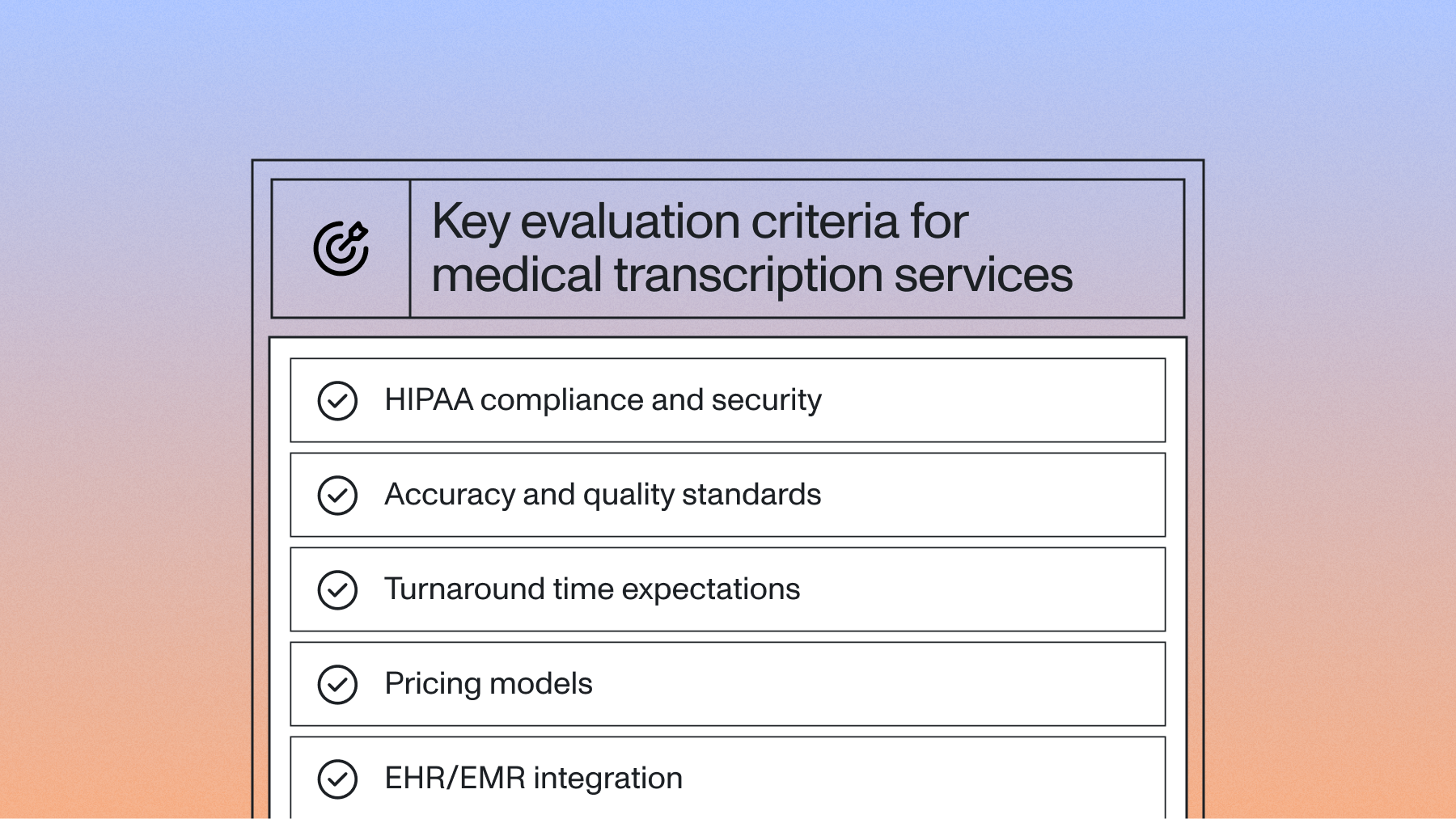
This guide compares the top 7 ambient AI scribe solutions for healthcare providers, covering key features, pricing, EHR integrations, and implementation considerations to help you choose the right documentation system for your practice.
Ambient AI scribes automatically capture and transcribe patient-provider conversations during medical visits, transforming spoken words into structured clinical notes without manual typing. This guide compares the top 7 ambient AI scribe solutions for healthcare providers, covering key features, pricing, EHR integrations, and implementation considerations to help you choose the right documentation system for your practice.
What is an ambient AI scribe
An ambient AI scribe is a Voice AI system that automatically captures and transcribes patient-provider conversations during medical visits. These systems listen to conversations through smartphones, tablets, or other devices placed in exam rooms and convert spoken words into structured clinical notes.
The technology works by recording the entire conversation between doctors and patients. Voice AI models then process this audio to identify different speakers and extract important medical information from the discussion.
Core components include:
- Speech recognition: Voice AI models convert spoken words into text, handling medical terms and natural conversation
- Speaker diarization: The system separates patient voices from provider voices to maintain proper context
- Clinical understanding: AI extracts medical information like diagnoses, medications, and symptoms from conversations
- Note generation: Automated creation of SOAP notes and other medical documentation formats
- EHR integration: Direct connection to electronic health records to save notes automatically
The process eliminates manual typing during patient visits. Doctors can focus entirely on patient care while the AI handles documentation in the background.
Top 6 ambient AI scribe solutions
1. Microsoft DAX Copilot
Microsoft DAX Copilot combines Nuance's medical speech recognition expertise with Microsoft's cloud infrastructure. The system captures conversations and generates clinical notes automatically within seconds after patient visits end.
DAX Copilot integrates deeply with Epic and other major EHR systems. The solution includes quality assurance reviews by medical documentation specialists.
Main features:
- Automated clinical documentation within EHR workflows
- Templates for over 40 medical specialties
- Mobile apps for iOS and Android
- Quality assurance by medical specialists
- Integration with Microsoft Teams for telehealth
Ideal for:
- Large health systems using Epic or supported EHRs
- Multi-specialty medical groups wanting standardized documentation
- Organizations prioritizing vendor stability and enterprise support
Pricing:
- Starts at $200 per provider monthly
- Enterprise pricing for large deployments
- Additional costs for quality assurance services
2. Ambience Healthcare
Ambience Healthcare's AutoScribe platform focuses on comprehensive ambient documentation with clinical decision intelligence features. The system provides real-time coding suggestions, quality measure tracking, and automated prior authorization support.
Their AutoCDI feature helps maximize reimbursement by ensuring complete documentation. The platform goes beyond basic transcription to offer revenue optimization tools.
Main features:
- AutoScribe for real-time clinical documentation
- AutoCDI for documentation improvement and coding optimization
- Specialty modules for emergency medicine, cardiology, orthopedics
- Real-time clinical decision support
- Automated referral letter generation
Ideal for:
- Multi-specialty practices focused on revenue optimization
- Academic medical centers requiring detailed documentation
- Specialty practices in complex fields like cardiology
Pricing:
- Custom enterprise pricing based on practice size
- Typically ranges from $300-500 per provider monthly
- Implementation and training services included
3. Athelas Ambient AI
Athelas combines ambient documentation with practice management features for independent practices. Their system integrates with over 20 EHR systems and includes voice commands for hands-free operation during procedures.
The platform emphasizes quick deployment with minimal training requirements. Athelas focuses on billing accuracy alongside documentation efficiency.
Main features:
- One-tap activation for instant documentation
- Voice commands for hands-free note editing
- Automated charge capture and billing optimization
- Patient instruction generation
- Integrated telehealth documentation support
Ideal for:
- Independent primary care and urgent care practices
- Physicians wanting quick implementation without IT resources
- Practices prioritizing billing accuracy with documentation
Pricing:
- $149 per provider monthly
- No setup fees or long-term contracts
- 14-day free trial available
4. Nabla
Nabla's Copilot offers an accessible entry point for practices exploring ambient documentation. The platform includes a generous free tier and supports over 30 languages for diverse patient populations.
The system generates notes in under 30 seconds after encounters end. Nabla works alongside any EHR system through its web interface.
Main features:
- Multi-language support for diverse communities
- Customizable note templates and formatting
- SOAP note generation with clinical summaries
- Patient instruction letters in multiple languages
- Web-based interface requiring no installation
Ideal for:
- Small practices and solo practitioners
- Clinics serving multilingual communities
- Providers wanting to test ambient documentation before committing
Pricing:
- Free tier with 30 consultations monthly
- Professional plan at $119 per provider monthly
- Enterprise pricing for larger organizations
5. Tali AI
Tali AI focuses specifically on the Canadian healthcare market with deep integration into Canadian EHR systems. The platform complies with provincial privacy regulations and includes Canadian medical terminology.
Tali works as a desktop assistant that runs alongside existing EHR systems. The solution combines ambient documentation with voice-enabled EHR navigation.
Main features:
- Voice-enabled EHR navigation and search
- Canadian medical terminology and billing code support
- Provincial privacy law compliance
- Medical reference search via voice commands
- Desktop-based solution for secure environments
Ideal for:
- Canadian family medicine practices
- Physicians using Canadian EHR systems
- Clinics requiring provincial regulatory compliance
Pricing:
- $129 CAD per provider monthly
- Annual billing discounts available
- 14-day free trial
6. Heidi Health
Heidi Health provides an affordable ambient scribe solution with a permanently free tier for providers seeing fewer patients. The platform offers extensive customization options for note templates and adapts to individual documentation styles.
Heidi's AI learns from corrections to improve accuracy over time. The system provides multiple note format options to match provider preferences.
Main features:
- Customizable documentation templates
- Learning algorithm that adapts to provider preferences
- Multiple note format options
- Basic billing code suggestions
- Web and mobile applications
Ideal for:
- Solo practitioners and small practices
- Providers wanting customizable documentation
- Practices with variable patient volumes
Pricing:
- Free tier for up to 10 consultations monthly
- Professional plan at $99 monthly
- Custom enterprise pricing available
8. Athenahealth Ambient Notes
Athenahealth's Ambient Notes comes integrated with their athenaOne EHR platform. The solution provides seamless documentation without requiring third-party integration.
The system automatically populates relevant EHR fields and suggests appropriate billing codes based on documented services. Integration eliminates workflow disruptions.
Main features:
- Native integration with athenaOne EHR
- Automatic field population in patient charts
- Suggested diagnosis and procedure codes
- Quality measure tracking and reporting
- Mobile and desktop compatibility
Ideal for:
- Current athenaOne customers
- Primary care practices using athenahealth
- Organizations seeking single-vendor solutions
Pricing:
- Included with athenaOne subscriptions
- No additional per-provider fees
- Available to all athenaOne customers
How ambient AI scribes transform healthcare documentation
Healthcare providers spend hours weekly on documentation, with much of this work happening after clinic hours. Ambient AI scribes change this by capturing clinical encounters automatically while physicians focus entirely on patient care.
The transformation begins when providers stop dividing attention between computer screens and patients. Eye contact returns to exam rooms, and conversations flow naturally without typing interruptions.
Key benefits include:
- Time savings: Providers save hours daily on documentation tasks
- Improved patient engagement: Increased eye contact and natural conversation during visits
- Reduced burnout: Elimination of after-hours charting and weekend documentation
- Better documentation quality: More comprehensive capture of clinical details and patient concerns
- Revenue optimization: Complete documentation supports appropriate coding and reduces claim denials
The technology restores the human connection in healthcare by removing the barrier of simultaneous documentation and patient interaction. Physicians report higher job satisfaction when they can focus on patient care rather than data entry. Physicians report higher job satisfaction when they can focus on patient care rather than data entry.
Key features of ambient AI scribes
Modern ambient AI scribes offer capabilities that extend beyond simple transcription services. These systems understand medical context, recognize clinical patterns, and generate documentation that meets regulatory requirements.
Core documentation features:
- Real-time transcription with minimal delay for live documentation
- Automatic SOAP note structuring without manual formatting
- Specialty-specific templates for different medical fields
- Multi-language support for diverse patient populations
Clinical intelligence capabilities:
- Medical Entity Detection for diagnoses, medications, allergies, and procedures
- ICD-10 and CPT code suggestions based on documented services
- Clinical decision support alerts for potential issues
- Quality measure tracking for reporting programs
Workflow integration options:
- Direct EHR write-back via standard healthcare data formats
- Mobile and desktop compatibility for flexible documentation
- Offline mode for areas with limited internet connectivity
- Team collaboration features for multi-provider encounters
The most advanced systems incorporate large language models to understand context and generate natural, comprehensive notes that capture the nuance of clinical conversations.
EHR integration and implementation considerations
Successful deployment of ambient AI scribes requires planning around technical infrastructure, security compliance, and workflow optimization. Organizations must evaluate their existing EHR capabilities and provider readiness before implementation.
Integration complexity varies significantly depending on the chosen solution and existing technology. Some solutions offer native EHR integration while others require API connections or third-party middleware.
Technical requirements include:
- API compatibility with existing EHR systems
- Network bandwidth for real-time audio streaming
- Device requirements including mobile compatibility
- Audio capture quality with noise cancellation
Security and compliance essentials:
- Business Associate Agreement execution for healthcare compliance
- Security certifications and audit capabilities
- Data retention policies aligned with regulations
- Access controls and user authentication
Training and adoption strategies:
- Provider onboarding covering activation and review workflows
- Workflow optimization to maximize efficiency gains
- Success metrics tracking including time savings and quality
- Change management support for hesitant adopters
AssemblyAI enables covered entities and their business associates subject to HIPAA to use the AssemblyAI services to process protected health information. AssemblyAI is considered a business associate under HIPAA, and offers a Business Associate Addendum that ensures appropriate safeguarding of patient information.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.