What is an Ambient AI Scribe and how do they work?
Medical documentation consumes hours of physician time daily, pulling focus away from patient care toward typing and note-taking—a problem driving the rapid growth of the $600 million ambient AI scribe market. Ambient AI scribes solve this problem by listening to natural conversations between doctors and patients, then automatically generating structured clinical notes without requiring any changes to your appointment workflow. These Voice AI systems work passively in the background, capturing medical discussions and transforming them into properly formatted documentation for electronic health records.
Understanding how ambient AI scribes function helps healthcare providers evaluate whether this technology fits their practice needs. This article explains the core components that power ambient AI scribes—from speech recognition through clinical understanding to documentation generation—plus the practical workflow, benefits, and implementation considerations that determine successful deployment in real healthcare environments.
What is an ambient AI scribe?
An ambient AI scribe is software that records medical appointments and creates clinical documentation automatically. Think of it as a smart assistant that listens to your patient conversations and writes notes for you. The word "ambient" means it works passively in the background—you don't need to speak directly to it or change how you normally conduct appointments.
Here's what makes ambient AI scribes different from older systems. Traditional medical transcription required you to dictate notes after seeing patients, often hours later when details were fuzzy. Voice recognition software made things faster but still demanded your active participation and frequent corrections.
Ambient AI scribes represent the next evolution. They combine multiple AI technologies to understand medical conversations, identify who's speaking, and create proper documentation without interrupting your workflow.
- Traditional transcription: You dictate detailed notes hours after appointments
- Voice recognition: You actively dictate while the system types, requiring corrections
- Ambient AI scribes: You conduct normal appointments while AI creates draft notes automatically
The technology handles complex medical terminology, distinguishes between different speakers, and understands clinical context without any input from you during the patient visit.
How ambient AI scribes work
Ambient AI scribes transform your spoken conversations into medical documentation through three connected stages. Each stage builds on the previous one, starting with capturing audio and ending with formatted clinical notes.
Speech recognition converts conversations to text
The first step is speech-to-text conversion using automatic speech recognition (ASR) technology. This AI model listens to your appointment and turns everything said into written text, handling the unique challenges of medical settings.
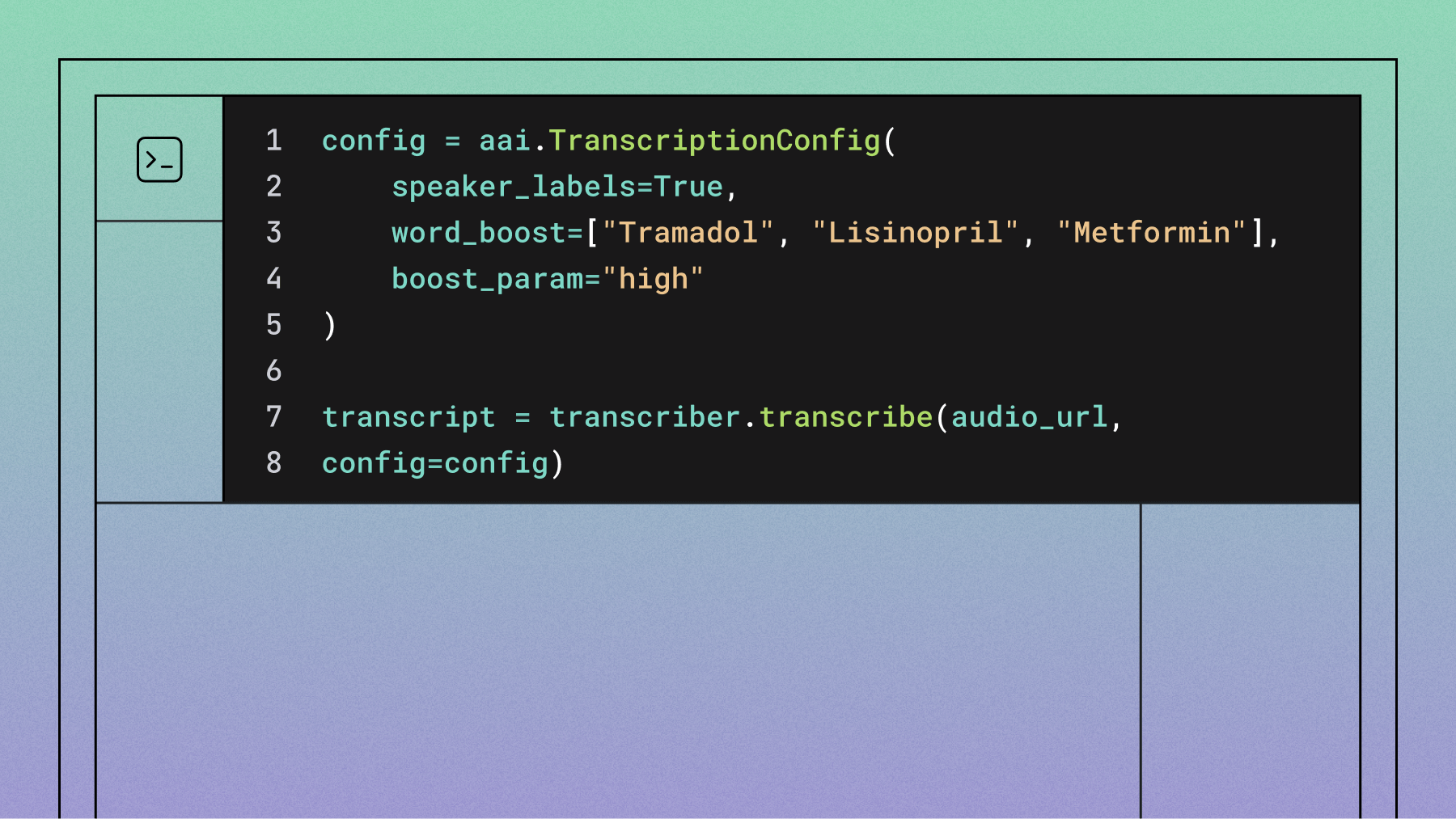
Medical speech recognition is more complex than general transcription. The system must recognize drug names like "lisinopril" and "metoprolol," understand medical abbreviations, and distinguish between multiple people talking. It also needs to work despite background noise from medical equipment, hallway conversations, and varying speech patterns.
The accuracy here determines everything that follows. If the system mishears "chest pain" as "test pain," the entire note becomes unreliable. Modern Voice AI models achieve high accuracy even with challenging audio conditions, but they're specifically trained on medical vocabulary and clinical scenarios.
- Medical terminology recognition: Accurately captures drug names, procedures, and anatomical terms
- Speaker diarization: Knows when you're talking versus your patient or family members
- Noise handling: Works despite equipment sounds and hallway distractions
- Accent adaptation: Understands diverse speech patterns from patients and providers
Natural language processing extracts clinical meaning
Once your conversation becomes text, natural language processing (NLP) analyzes the transcript to extract medical meaning. This goes far beyond simple transcription—the AI understands medical context and relationships between different pieces of information.
The system recognizes that when you say "SOB," you mean shortness of breath, not something inappropriate. It connects symptoms with timing, medications with dosages, and current problems with medical history. Advanced models understand when you're discussing active issues versus past medical history, or confirmed diagnoses versus differential considerations.
This stage identifies clinical entities like symptoms, medications, diagnoses, and procedures while mapping their relationships. If a patient mentions starting chest pain "two weeks ago," the AI connects that timing with the symptom even if they're mentioned in different parts of the conversation.
Documentation generation creates structured notes
The final stage transforms extracted clinical information into properly formatted medical documentation. The AI organizes conversation elements into standard note templates like SOAP format, populating each section with relevant details from your appointment.
The system suggests appropriate billing codes, identifies follow-up requirements, and formats everything according to your specialty's documentation standards. But here's the crucial part—this creates a draft, not a final document. You always review and approve every note before it goes into the patient record.
You can edit any section, verify accuracy against the original audio, and ensure the documentation reflects your clinical judgment. The AI handles the mechanical work of organizing and formatting, while you maintain complete control over the medical content.
Test speech-to-text accuracy in the Playground
Upload sample audio and experiment with transcription, speaker diarization, and formatting. See how accurate models handle multi-speaker conversations before you build.
Try the playground
Clinical workflow from encounter to documented note
Using an ambient AI scribe follows a simple workflow that fits naturally into your existing practice. Understanding this process helps you see how the technology integrates without disrupting your patient care routine.
You start each appointment by getting verbal consent from your patient for AI-assisted documentation. While this isn't legally required everywhere, it builds trust and gives patients the option to decline without affecting their care quality.
Next, you conduct your appointment exactly as you normally would. The ambient AI scribe records through a smartphone app or dedicated device, but you don't need to think about it. You focus entirely on your patient—making eye contact, asking questions, performing examinations—while the AI captures everything in the background.
As soon as you end the recording, the AI processes the audio through all three stages we just discussed. Within one to two minutes, you have a complete draft note ready for review. This happens fast enough that you can approve it before seeing your next patient.
- Patient consent: Brief verbal request to use AI documentation assistance
- Normal appointment: Conduct your visit without any changes to your routine
- Instant processing: AI creates draft notes within minutes of ending the recording
- Quick review: Edit and approve the note before moving to your next patient
- Automatic integration: Approved note uploads directly to your EHR system
The original audio recording gets deleted after a brief retention period for quality assurance, protecting patient privacy while ensuring the system can improve over time.
What are the benefits of ambient AI scribes?
Ambient AI scribes deliver three major improvements to your practice: time savings, reduced burnout, and better patient connections. These benefits emerge from removing documentation burden from your clinical encounters.
Time savings transform your schedule—The Permanente Medical Group documented 15,791 hours saved in one year, equivalent to 1,794 eight-hour workdays. Instead of spending hours completing notes after work—what many doctors call "pajama time"—you finish documentation immediately after each patient visit. This efficiency lets you either see more patients or leave work on time, depending on your practice needs.
Burnout reduction comes from eliminating documentation stress. The constant pressure of note-taking contributes significantly to physician burnout and job dissatisfaction. When ambient AI scribes handle the mechanical aspects of documentation, you feel more energized and satisfied with your work.
Enhanced patient engagement restores the human connection in healthcare. You maintain eye contact, observe non-verbal cues, and engage in deeper conversations when not distracted by computer screens. Patients feel heard and valued when your full attention focuses on them rather than typing.
The compound effect of these benefits extends beyond individual appointments. When you're less stressed about documentation, you communicate better with patients. When patients feel more engaged, they provide better information and follow treatment plans more consistently.
Some doctors report that ambient AI scribes improve their diagnostic abilities. Without the distraction of note-taking, you notice subtle cues in patient behavior, speech patterns, and physical presentation that might otherwise be missed while typing.
Challenges and considerations
While ambient AI scribes offer substantial benefits, you should understand several implementation challenges before deploying this technology in your practice.
Accuracy varies with environmental conditions. Clinical settings present unique challenges for speech recognition. Emergency departments have constant background noise, exam rooms may echo, and multiple people often speak simultaneously. Even advanced Voice AI models can struggle with heavily accented speech, elderly patients with soft voices, or rapid medical discussions between specialists.
Integration complexity affects implementation timeline. Ambient AI scribes must connect with your existing EHR system, comply with healthcare IT standards, and fit into established workflows. This integration requires technical expertise and often custom configuration for your specific healthcare system.
Physician adoption isn't universal. Not all doctors embrace ambient AI scribes equally. Some worry about accuracy, others prefer their established documentation methods, and many need training to trust AI-generated notes. Successful implementation requires change management strategies and physician champions who can demonstrate value to skeptical colleagues—research shows that establishing multidisciplinary AI committees with iterative pilots improves workflow efficiency and clinician satisfaction.
Privacy and compliance demand robust security. Healthcare data requires the highest protection standards. Ambient AI scribes must ensure end-to-end encryption, secure data transmission, and compliance with healthcare regulations. You need clear policies about data retention, patient consent procedures, and audit trails.
The technology also requires reliable internet connectivity for cloud-based processing. Practices in areas with poor connectivity may experience delays or processing failures that disrupt workflow efficiency.
Final words
Ambient AI scribes transform clinical documentation by capturing natural conversations between you and your patients, then automatically generating structured medical notes through advanced Voice AI technology. This workflow—from speech recognition through clinical understanding to formatted documentation—frees you from typing during appointments while maintaining complete control over your medical records through review and approval processes.
The success of ambient AI scribes depends on robust speech-to-text technology that accurately captures medical conversations across diverse clinical environments. AssemblyAI's Voice AI models provide the foundational accuracy needed for reliable healthcare documentation, handling complex medical terminology, multiple speakers, and challenging audio conditions that are common in clinical settings.
Building an ambient AI scribe?
Get the complete guide to evaluating Voice AI for healthcare—covering clinical accuracy, speech understanding, HIPAA compliance, and the technical capabilities that matter most.
Read the guide
Frequently asked questions
Do patients need to consent before ambient AI scribe recording starts?
Yes, obtaining verbal consent is considered best practice even without a federal mandate. This transparency builds patient trust and respects their autonomy to decline AI assistance without affecting care quality.
How quickly do ambient AI scribes generate clinical notes after appointments?
Most systems generate draft notes within one to two minutes after you end the recording. This near-instantaneous processing allows you to review and approve documentation immediately after patient visits.
What happens when the ambient AI scribe makes transcription errors?
All AI-generated notes are drafts requiring your review and approval before finalization. You can view original transcripts, play audio segments, and edit any content to ensure complete accuracy before the note enters your patient's medical record.
Can ambient AI scribes identify multiple speakers during patient encounters?
Yes, speaker diarization technology distinguishes between different voices and correctly attributes statements to each speaker, labeling them as Speaker A, Speaker B, and so on. The technology works best with two to four speakers in clear audio conditions. Some systems, like AssemblyAI's Speaker Identification feature, can take this further by mapping these generic labels to specific names or roles (such as you, your patient, and family members) when provided with that information.
Do ambient AI scribes work with specialty-specific medical terminology?
Modern ambient AI scribes are trained on medical vocabulary from multiple specialties, recognizing terms specific to cardiology, orthopedics, psychiatry, and other fields. However, highly specialized practices may need additional customization for optimal accuracy.
What happens to the original audio recordings after note generation?
Audio recordings are permanently deleted after a brief retention period used for quality assurance and system improvement. This automatic deletion protects patient privacy while allowing the AI system to learn from real-world usage patterns.
Title goes here
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.