Medical terminology accuracy: Techniques for domain-specific transcription
Medical transcription accuracy is critical for reliable clinical documentation, patient safety, and compliance. Learn how to reduce errors and improve outcomes.
Medical transcription accuracy determines whether AI systems correctly capture critical clinical information when doctors dictate patient notes, as medication errors rank as the most frequent and avoidable source of patient harm. Standard accuracy metrics like Word Error Rate treat every word equally, but in healthcare, confusing "15 milligrams" with "50 milligrams" creates life-threatening consequences that a simple percentage can't capture.
Healthcare organizations need transcription systems that understand the difference between harmless grammatical errors and dangerous clinical mistakes. This article explains how medical transcription accuracy gets measured, what types of errors create the biggest patient safety risks, and proven techniques for achieving reliable clinical documentation that protects both patients and healthcare providers from preventable harm.
How is medical transcription accuracy measured?
Medical transcription accuracy is how precisely spoken medical content gets converted to written text. This means measuring how often an AI system correctly captures medication names, dosages, symptoms, and diagnoses when doctors dictate patient notes. But here's the thing: the standard metrics that vendors use to advertise their accuracy don't tell you the whole story about clinical safety.
Most companies measure accuracy using Word Error Rate (WER), which calculates the percentage of incorrectly transcribed words. Character Error Rate (CER) measures character-level mistakes. These metrics treat every word equally, whether it's a filler word like "um" or a critical medication dosage that could harm a patient if transcribed wrong.
Think about this: a transcript could have a WER showing it's accurate, but if it changes "15 milligrams of morphine" to "50 milligrams of morphine," you're looking at a potentially fatal overdose. That's one wrong number in hundreds of correct words, but the clinical consequence is massive.
Word Error Rate vs clinical accuracy
Word Error Rate uses this formula: (Wrong words + Missing words + Extra words) ÷ Total Words × 100. A system with accuracy sounds impressive—only 2 out of every 100 words are wrong. But what happens when those two words completely reverse a diagnosis?
Here's why WER doesn't capture clinical risk:
- Equal weight fallacy: Missing "no" in "no known allergies" gets the same error score as missing "um"
- Context blindness: Changing "hypertension" to "hypotension" reverses the entire treatment plan
- Decimal disasters: Shifting 1.5mg to 15mg is a tiny character change but a massive dosing error
Clinical accuracy weighs errors by their potential harm to patients. A grammatical mistake that doesn't change meaning matters far less than a drug name substitution that could trigger an allergic reaction.
Why accuracy claims can be misleading
Vendors test their systems under perfect conditions like clean audio, standard accents, common medical terms. Your real-world environment doesn't look like their testing lab. You've got beeping monitors, conversations happening nearby, physicians dictating while walking down hallways, and international doctors with various accents.
The performance gap between marketing claims and reality can be shocking:
- Cherry-picked conditions: Testing with studio-quality audio and slow, clear speech
- Limited vocabulary: Using only common medical terms, not rare drug names or new procedures
- Accent bias: Testing primarily with American English speakers
- Noise-free environments: Ignoring the reality of busy clinical settings
A system claiming accuracy in controlled tests might drop to accuracy when dealing with real emergency department conditions.
What errors occur in AI medical transcription?
Medical transcription errors fall into four categories that create specific risks in healthcare settings. Each type poses different challenges for detection and poses unique dangers to patient safety.
Substitution errors replace correct words with wrong ones. Omission errors delete critical words entirely. Insertion errors add words that weren't spoken. Speaker attribution errors assign statements to the wrong person.
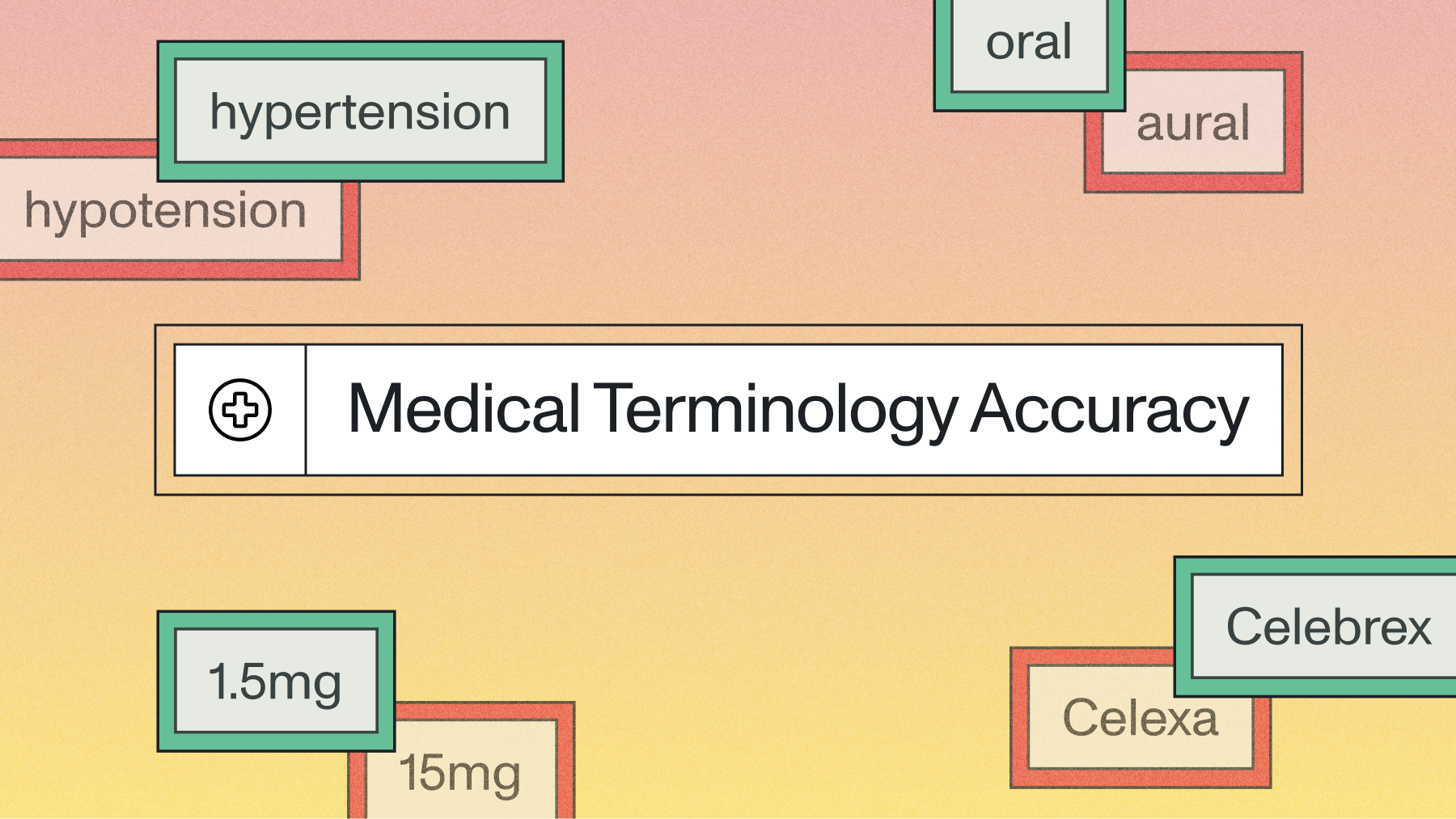
Substitution errors with medical terminology
Medical vocabulary creates dangerous homophones and similar-sounding terms that AI systems frequently confuse. "Hypertension" and "hypotension" sound nearly identical but represent opposite conditions requiring completely different treatments.
Drug name confusion poses the biggest immediate danger:
- Similar medications: "Celebrex" (anti-inflammatory) becomes "Celexa" (antidepressant)
- Dosage disasters: "Fifteen" becomes "fifty" or "point five" becomes "five"
- Route confusion: "Oral" becomes "aural" (by mouth vs. by ear)
These substitutions happen more frequently when physicians dictate quickly while multitasking or when dealing with accented speech that the AI model hasn't encountered during training.
Omissions in clinical documentation
Missing words create the most dangerous errors because they're harder to spot during review. When "no signs of malignancy" becomes "signs of malignancy," the sentence reads smoothly but conveys the opposite clinical meaning.
Omitted negations represent the highest risk:
- Symptom reversals: "No fever" becomes "fever"
- Finding opposites: "No abnormalities" becomes "abnormalities"
- Medication status: "Discontinued" gets dropped, suggesting ongoing treatment
- Time qualifiers: Missing "yesterday" or "last month" changes timeline context
These omissions often occur with short, unstressed words that AI models miss when physicians speak rapidly between patient visits.
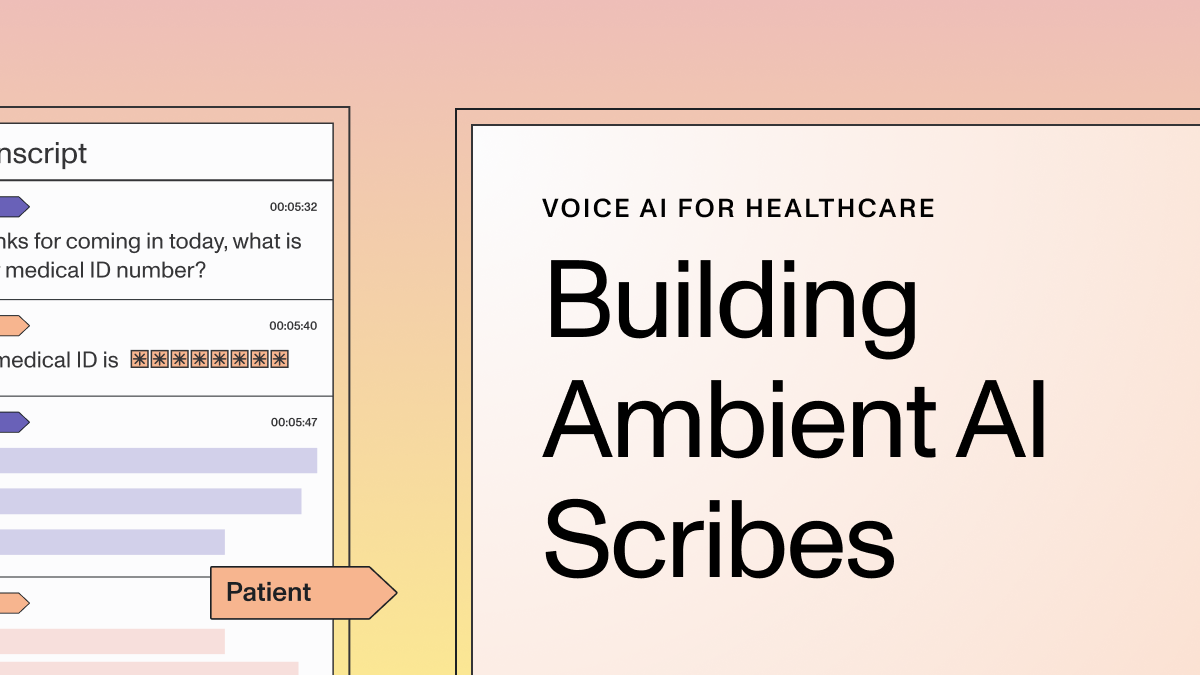
Speaker attribution and diarization failures
Speaker diarization identifies who said what during medical encounters with multiple participants. When family members provide medical history, their statements getting attributed to the patient creates fundamentally incorrect medical records.
Picture this scenario: A daughter says "She gets confused sometimes" about her elderly mother, but the transcript attributes this statement to the patient saying "I get confused sometimes." The clinical picture changes completely.
These attribution errors multiply in teaching hospitals where medical students, residents, nurses, and attending physicians all contribute to patient discussions. Getting attribution wrong means important clinical information gets misassigned or overlooked entirely.
What are the consequences of transcription errors?
Transcription errors create cascading problems throughout healthcare systems. A single mistake triggers chains of medical errors, legal complications, and administrative headaches that affect patient safety and organizational liability.
Patient safety and clinical outcomes
Medication errors from transcription mistakes harm patients regularly. When a physician dictates "Start metoprolol 25mg daily" but the transcript reads "250mg daily," that's a dose that could cause dangerous drops in heart rate and blood pressure.
Diagnostic cascades represent another serious consequence. Transcription errors that suggest nonexistent conditions lead patients through unnecessary medical workups:
- False positive findings: Omitted "no" triggers unneeded cardiac testing
- Wrong medication orders: Incorrect drug names cause allergic reactions
- Surgical site errors: Misheard "left" vs "right" leads to wrong-site procedures
- Delayed diagnoses: Critical findings get buried in transcription mistakes
Each error doesn't just affect one patient—it consumes healthcare resources, creates anxiety for families, and exposes organizations to malpractice liability.
Legal and regulatory implications
Medical records serve as legal documents in malpractice lawsuits, disability claims, and insurance disputes. Inaccurate transcription undermines physicians' legal defenses when their documented notes don't match their clinical reasoning.
Courts treat medical records as the definitive account of patient care. If the transcription contains errors, the legal record becomes unreliable for defending medical decisions or establishing timelines of care.
- Malpractice vulnerability: Wrong documentation undermines defense strategies
- Billing fraud risks: Incorrect procedure codes trigger Medicare audits
- Regulatory compliance: Documentation errors violate Joint Commission standards
- Insurance disputes: Wrong diagnostic codes affect claim processing
Healthcare organizations face penalties ranging from payment clawbacks to criminal investigations when transcription errors create patterns of incorrect billing or documentation that violate Joint Commission standards.
How do you ensure medical transcription accuracy?
Achieving reliable medical transcription requires multiple layers of quality control that combine AI efficiency with human medical expertise. No single approach eliminates all errors, but a comprehensive strategy reduces mistakes to clinically acceptable levels.
The most effective approach uses AI for initial transcription speed, then applies human medical knowledge for error detection and correction. This hybrid model catches context-dependent mistakes while maintaining operational efficiency.
Human-in-the-loop verification
One approach is to combine AI's transcription speed with trained medical professionals reviewing and correcting errors before documents become permanent records. This approach catches the subtle medical context errors that AI systems miss.
A tiered review system allocates human attention where it matters most:
- High-risk documents: Surgical notes and discharge summaries get full human review
- Routine visits: Follow-up appointments use spot-checking based on confidence scores
- Administrative notes: Non-clinical content gets automated processing with exception handling
Medical transcriptionists familiar with clinical terminology can spot dangerous errors like drug name confusions or anatomical mix-ups that general reviewers might miss.
Real-time accuracy monitoring
Modern Voice AI systems provide confidence scores that flag uncertain transcriptions for human review. When the AI encounters unclear audio, unfamiliar medical terms, or ambiguous context, it signals low confidence rather than making potentially dangerous guesses.
Confidence scoring helps you focus quality assurance attention on segments most likely to contain errors:
- Low confidence alerts: System flags uncertain words for review
- Terminology tracking: Monitor performance on specialty-specific vocabulary
- Error pattern analysis: Identify recurring mistakes for model improvement
- Performance degradation: Detect when accuracy drops due to environmental changes
This real-time feedback allows immediate correction of problems before they affect multiple patient records.
Domain-specific model validation
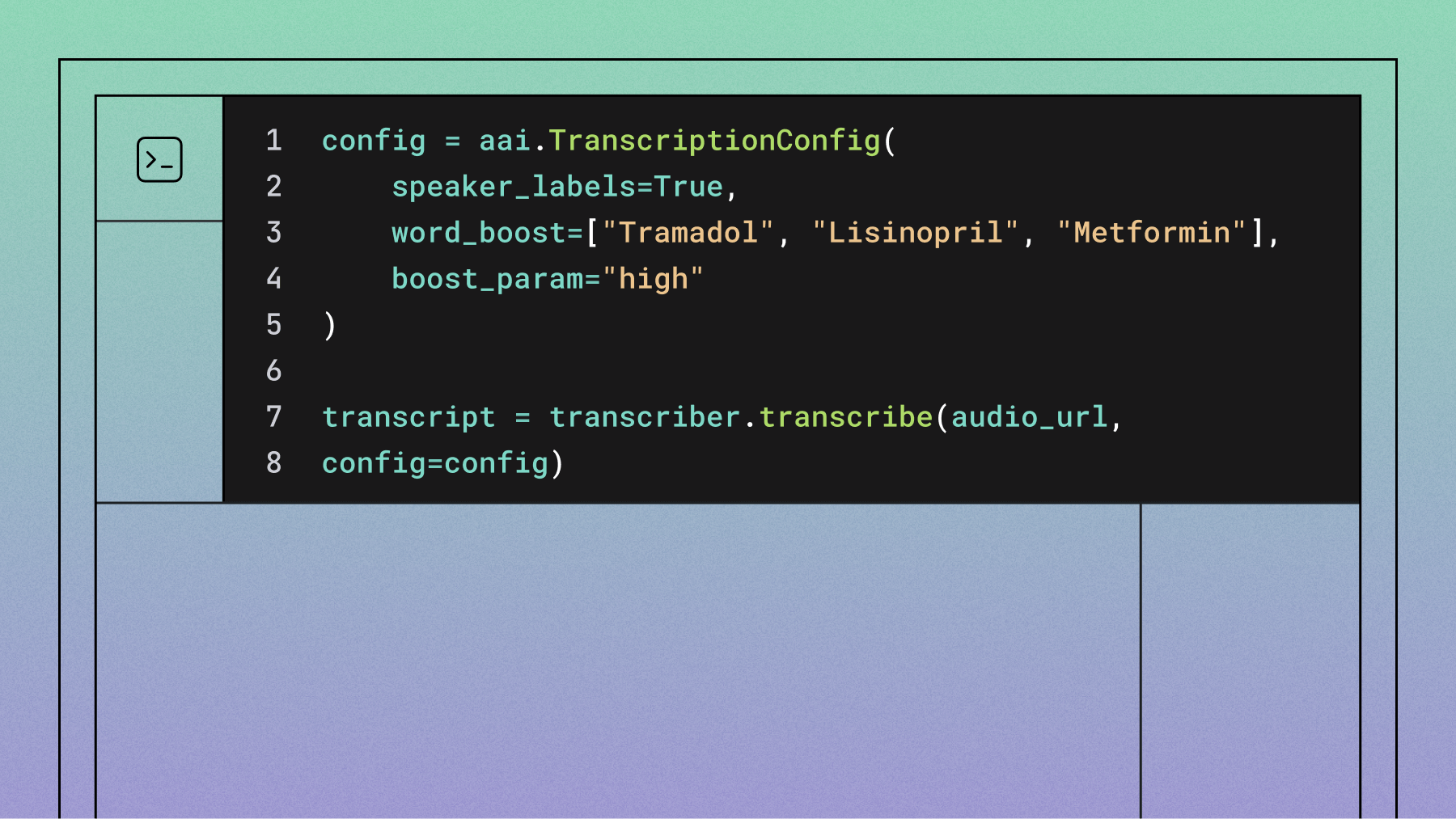
Generic transcription systems struggle with medical vocabulary, making specialized validation essential for healthcare applications. You need to test transcription performance against real medical terminology, including drug names, anatomical terms, and specialty procedures.
Effective validation covers challenging but common clinical scenarios:
- Specialty terminology: Test with cardiology, oncology, and surgical vocabulary specific to your practice
- Accented physicians: Validate performance with international medical graduates
- Background noise: Test accuracy with typical clinical environment sounds
- Rapid dictation: Measure performance when physicians speak quickly between patients
Voice AI systems designed for healthcare complexity can handle institution-specific vocabulary, physician name recognition, and local medical conventions that generic models miss.
Final words
Medical transcription accuracy demands understanding how different error types threaten patient safety and implementing quality assurance that combines AI efficiency with human medical expertise. The most successful approach treats transcription as an ongoing process requiring constant monitoring, error pattern analysis, and workflow adjustment based on real-world performance.